Please visit our new and updated site by clicking here.
Learn the technique .....
Page 2
Comments
Vaginal hysterectomy is the least invasive method of removal of uterus. Most of hysterectomies may be
performed vaginally.The lower rate of vaginal hysterectomy is not only due to the relative
contraindications to the vaginal route of hysterectomy but also due to the technical barriers in the mind
of most surgeons to deal with inadequate accessibility, poor visibility and effective hemostasis even
after considerable experiences.That is why they prefer a more obvious and widely visible abdominal
or laparoscopic route of hysterectomy even for a moderate size uterus.Our goal should be to perform the
vast majority of hysterectomies for benign disease via the vaginal route.
Only detachment of the lateral attachments was enough to remove uterus in majority (86.45%) of cases.
Debulking was needed in only 13.55% cases when Purohit technique was used.
Failure is very rare(<1%).
We have performed over 4000 vaginal hysterectomy by Purohit technique ( PTVH).
How to achieve adequate visibility during vaginal hysterectomy.
Incision of anterior vaginal wall by monopolar current
Incision on the anterior vaginal wall is
given by a frequent gentle stroke sufficient to expose the wall of cervix.
A deeper incision will incise the superficial part of myometrium and will go beyond the line of cleavage.
It will resemble a strong band of adhesion in the midline and will cause dissection problem.
Little superficial incision on the other hand will fall short of reaching line of cleavage.
Forceful dissection through this wrong plane will hit the bladder wall and will result in penetration
of lumen of bladder.
(The modified method, described in the operation procedures eliminates the problems of finding cleavage.)
The anterior margin of incision is lifted by an Alli's forceps when the incision falls short of
line of cleavage.The stretched taught tissue between the cut margins (Supravaginal septum or
vesicovaginal septum) is gently incised by a curved scissors directing its curvature against the a
nterior wall of cervix to get the cleavage to enter to the vesicocervical space.
When the incision goes beyond the line of cleavage, the adhered superficial layer of cervix to anterior
incision is treated as a strong band of adhesion and dissected later on by lateral approach.
Moreover, the complex anatomy around the uterine cervix needs a systematic approach to prevent most
complications.
Dissection of vesicocervical space and separation of bladder from cervix.
Vesicocervical space is bounded anteriorly by bladder, posteriorly by uterus and cervix, laterally
by bladder pillars, below by supravaginal septum and above by vesicouterine peritoneum.
It contains loose fascia. Normally bladder is peeled easily and quickly from the cervix by finger dissection.
If adhesions are sensed by finger during dissection, they are divided by sharp dissection.
Dissection is stopped on sensing a strong band of adhesion. No strong force is applied to detach it.
Usually these bands are thin and found in the lower boarder of vesicovaginal space.
The space above the scar is soft and can be easily pushed by finger.
By a lateral approach index finger is pushed lateral to the scar band to reach the upper part of
the vesicocervical space.The upper space is dissected by medially bend index finger and the band is isolated.
It is then 'hooked' by the finger.We prefer to 'hook' it by the bend of a right angle forceps (Figure 1)
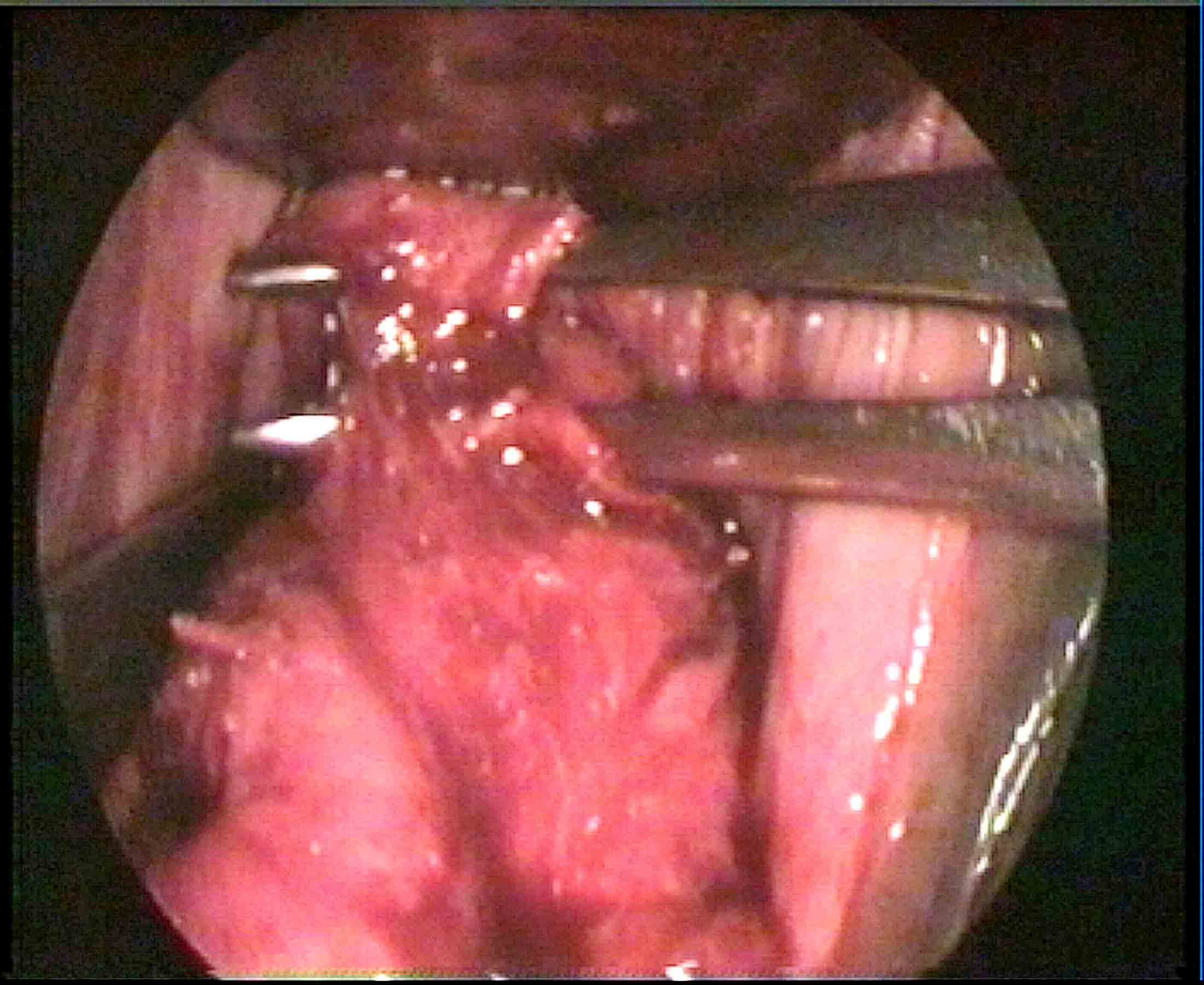
Figure - 1
Opening of posterior Pouch:
Choice of forceps with energy for vaginal hysterectomy
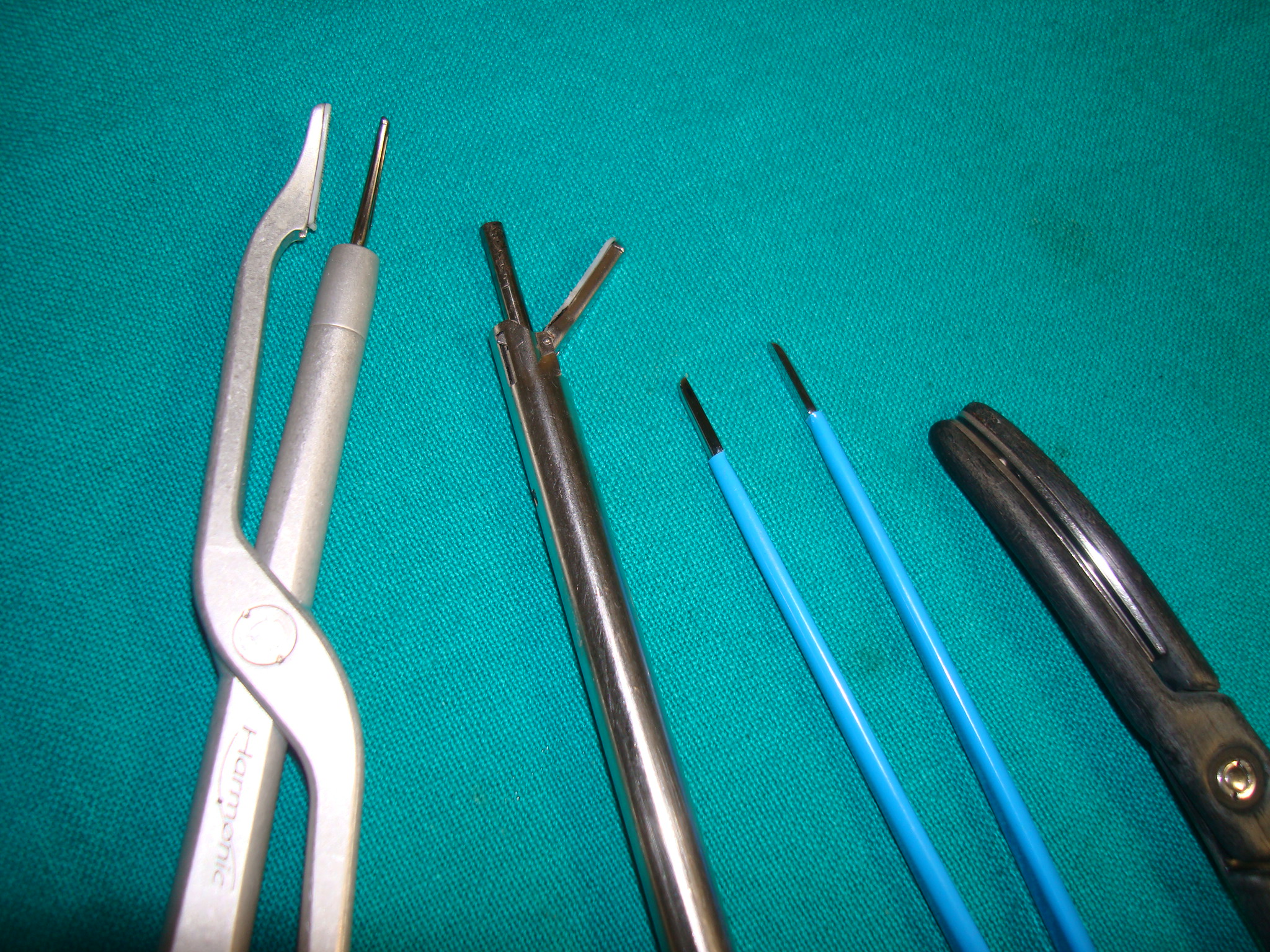
Figure 2 (compares thickness of tips of forceps)
Bipolar forceps alone may be used throughout.It has thin tip. Bipolar may be combined with Bi clamp forceps. Use bipolar forceps up to the level of uterosacral ligament. Above level of uterosacral we get wider space and use bi clamp.Bi clamp has thick tip. At the end, we again use bipolar forceps for effective hemostasis of tiny vessels. Similarly, we use thick Harmonic (focus and wave) forceps when available space is wide. Scissors is usually not needed when Harmonic focus is used. Postoperative pain is less in cases after harmonic than after bipolar. Similar to bipolar forceps, three strokes of harmonic forceps (at level -1 setting) along the length of uterine artery seals the uterine artery stump. We keep bi polar ready in case harmonic does not seal the vessel. However, all forceps are used between prongs of right angle forceps to improve the safety and success of vaginal hysterectomy(Figure 3).
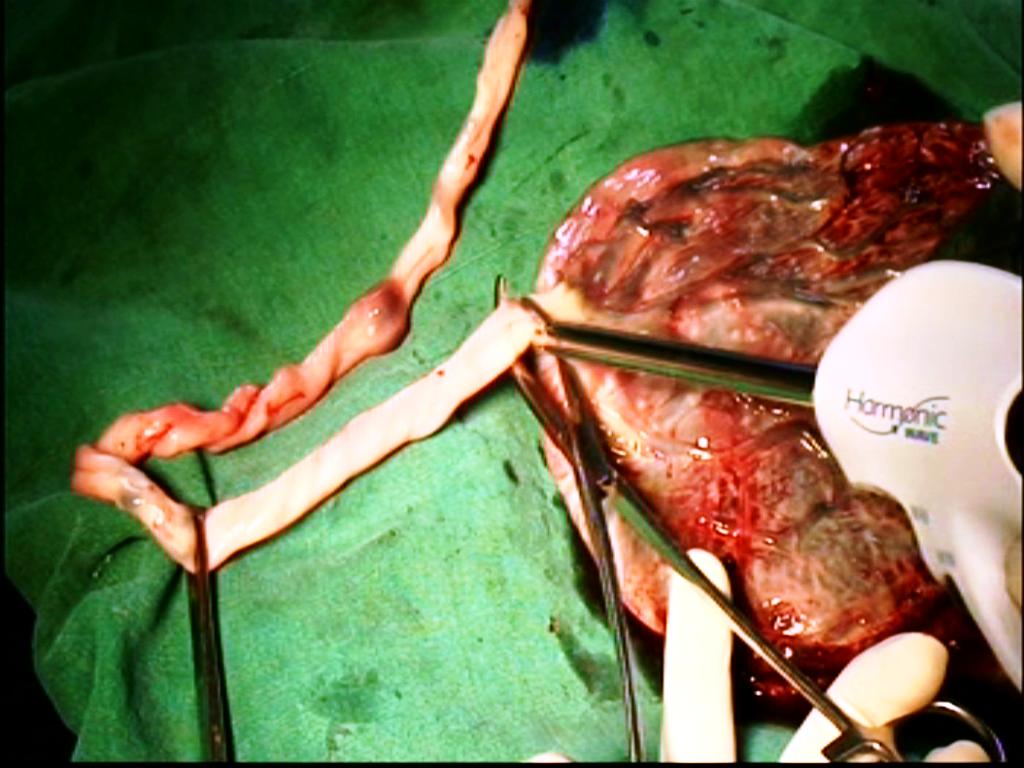
Bipolar,Bi clamp and Harmonic wave -placenta Model
Detachment of adhesions.
How to suspect clinically fundal adhesion to anterior abdominal wall scar.
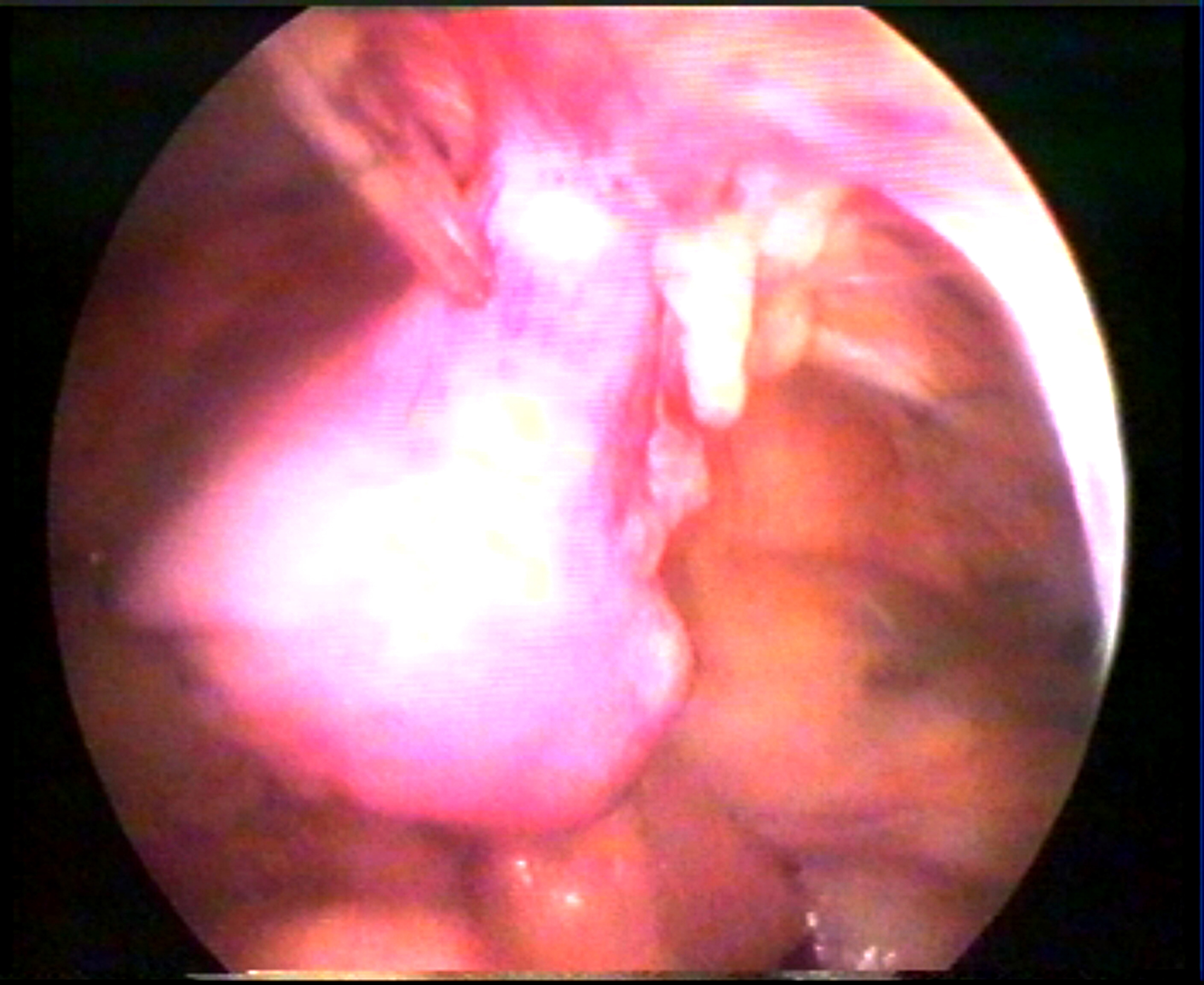
Figure 4 Fundal adhesion to anterior abdominal wall.
How to achieve effective hemostasis during vaginal hysterectomy.
Traditionally ligaments are clamped, detached, and transfixed by suture when space is wide.The ends are held long for fixation to the vault at the end of operation.Clampless technique is practiced when the space is inadequate. Use of a thick clamp, insertion of a curve needle lateral to the upper end of clamp and needle retrieval from posteriolateral aspect of the thick clamp require a wide space.It is troublesome when space is still inadequate. Moreover, a chance of ligature slippage causes apprehension of bleeding.In Purohit technique, ligaments are shaved from the cervix after bipolar coagulation (coagulation -and -cut maneuvers) close to cervix. It reduces chances of hemorrhage and ligature slippage.Ligaments are approached extraperitoneally.Tip of a right angle forceps is used to elevate the cervix from the posterior aspect to bring the target tissue to the operator's view before their coagulation and division.The coagulation -and -cut maneuvers need about 4 mm space.Thus, this technique is helpful in all cases with poor access.In our experience, lower ligaments of all cases with benign disease of uterus can be detached by Purohit technique.The forceps used in modern techniques of hemostasis like bipolar and harmonic etc need a straight passage to the target organ, and thus require less space than the ligature technique of hemostasis.When other forceps fail, bipolar forceps works thus always keep the bipolar forceps during vaginal hysterectomy.In Purohit technique, use of a right angle forceps further increases safety of the neighboring structures.Traction by the assistant is not so much required in our technique because tip of right angle forceps is used by left hand to elevate the ligaments from the posterior aspect for easy application of bipolar forceps by right hand.That reduces the tiredness of the assistant and postoperative pain of patient.The released Mackenrodts ligament does not retract back in any case in this extraperitoneal technique.We found that the difficulty of application of thick clamp and needle holder with needle in such cases of poor access in conventional method could be solved by our technique.Therefore, cases with poor access were not a contraindication in our technique.
Correctly, applied ligature is a time tested reliable method of hemostasis if the space is wide for ligature application.Clamp less technique used when the space is inadequate.When the space is still narrow then the modern hemostatic techniques like bipolar energy,ultrasonic energy, electrosurgical bipolar vessel sealer (EBVS) are used. When the distance between the ureter and cervix is <0.5 cm then the chance of ureteral injury relatively increases during hysterectomy.Isolation of uterine artery rather than bundle inclusion is a vital step to avoid coagulation injury to the neighboring structure.Purohit technique is different specially in showing advantages of use of a right angle forceps in isolating the uterine artery extraperitoneally. The right angle forceps creates space for bipolar forceps and scissors between its opened prongs and protects the neighboring structures from thermal injury.In this extraperitoneal technique, a bleeding uterine artery protrudes towards the surgeon than it retracts.A bleeding artery can be easily grasped by artery forceps and cauterized extraperitoneally.In this intraperitoneal technique, blood does not enter in to the peritoneal cavity during the procedure and bowels do not protrude on to the operation field.In the intraperitoneal technique in contrast, blood enters the peritoneal cavity, bowels come on the way of operation, the lower ligament, and uterine artery stumps recoil back to the lateral pelvic wall immediately after separation from cervix and uterus.It is some time difficult to trace a bleeding uterine vessel in the intraperitoneal approach to uterine artery.In our experience, uterine arteries can be secured extraperitoneally bilaterally in all cases of benign disease of uterus up to 16 weeks size of gestation.We have not encountered a case of postoperative hemorrhage from uterine artery.We believe bipolar method of hemostasis is reliable, safe, effective, and cheap in vaginal hysterectomy.Achievement of complete physical compression of the lumen (coaptation) of artery by prongs of bipolar forceps is a prerequisite before activating bipolar current.Bipolar needs 2-3 applications along the length of uterine vessel for complete hemostasis. We have not seen an avulsed stump postoperatively. Purohit approach to uterine artery is an easier and quicker approach to access, identify, dissect,and skeletonise the uterine artery even in cases of rotated and distorted uterus due to myoma.Its desiccation under direct vision between the prongs of right angle forceps further increases confidence and reduces intraoperative hemorrhage and chances of injury to ureter.
Traction is given on the round ligament and the stumps are exposed.The bipolar method of hemostasis is also reliable for the upper pedicles.Bipolar forceps is preferable in cases with narrow lateral space resulting from expanded uterine fundus and pelvic adhesions.Pelvic illuminator may be used in cases with poor visibility.
How to check
effective intraoperative hemostasis during vaginal hysterectomy by electrosurgery.
In Purohit technique, posterior
leaf of broad ligaments is routinely climbed up bilaterally up to the infundibulopelvic ligament to trace bleeder
if any from the lateral wall to prevent postoperative vault hematoma.Intraoperatively bleeding occurs from three
sites: (1) from the veins and arterioles of Mackrnodt's ligament, (2) from the ovarian pedicles and occasionally
from a tiny vessel below round ligament,and (3) from uterine artery.To deal with the bleeding from upper pedicles,
trace the pedicles by the technique described above, pull them down, and coagulate them properly.Use pelvic i
lluminator if needed to improve visibility.To deal with the uterine artery bleeding- trace it by the tracing
technique described above.Use the pelvic illuminator if needed to improve visibility.Then hold the bleeding stump by
an artery forceps.Use suction cannula to aspirate the blood. Lavage with normal saline.Now, cauterize the artery
proximal to the artery forceps.Well-cauterized artery is reliable postoperatively.Do not use suture.For bleeding from
Mackrnodt's ligament, hold the lateral vaginal wall by Allis forceps,pull it laterally to find any bleeding artery,
and cauterize it.In the absence of arteriolar bleeding, retrieve the uterosacral stump and then fix it to the lateral
vaginal wall.It will compress and stop the venous bleeding that cannot otherwise be cauterized.No time is wasted in
catching the venous bleeding from in side the ligament tear.Primary postoperative bleeding if any from the lateral
wall can also be traced and secured by this technique safely after opening vaginal vault with out affecting security
of other stumps.
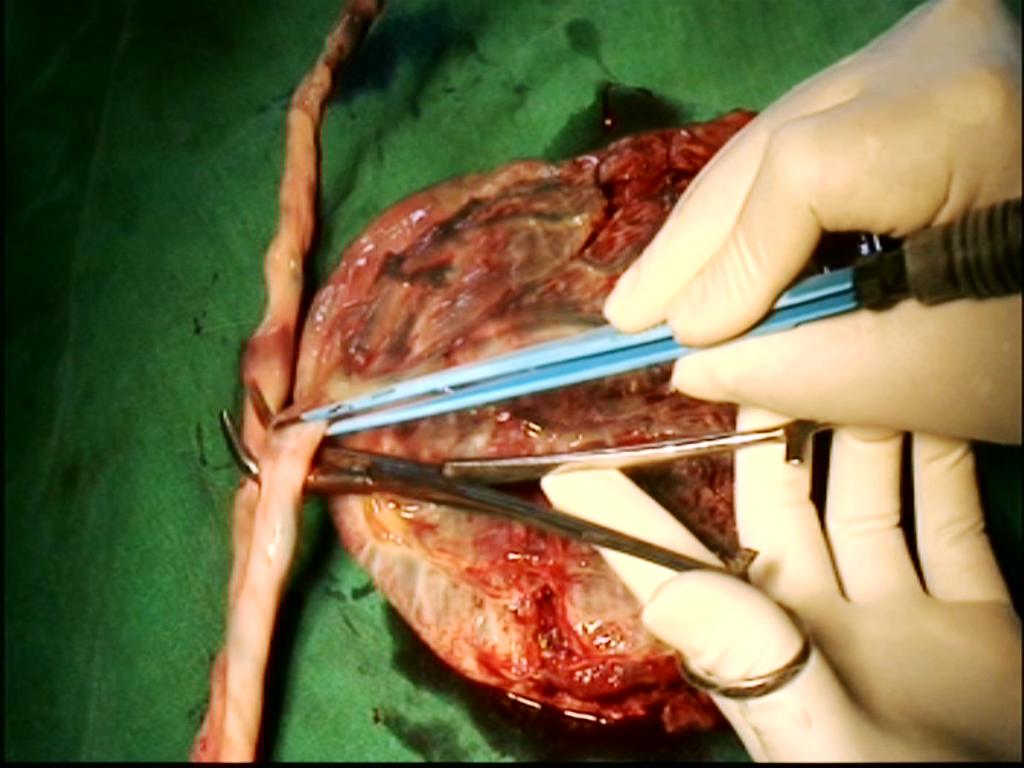
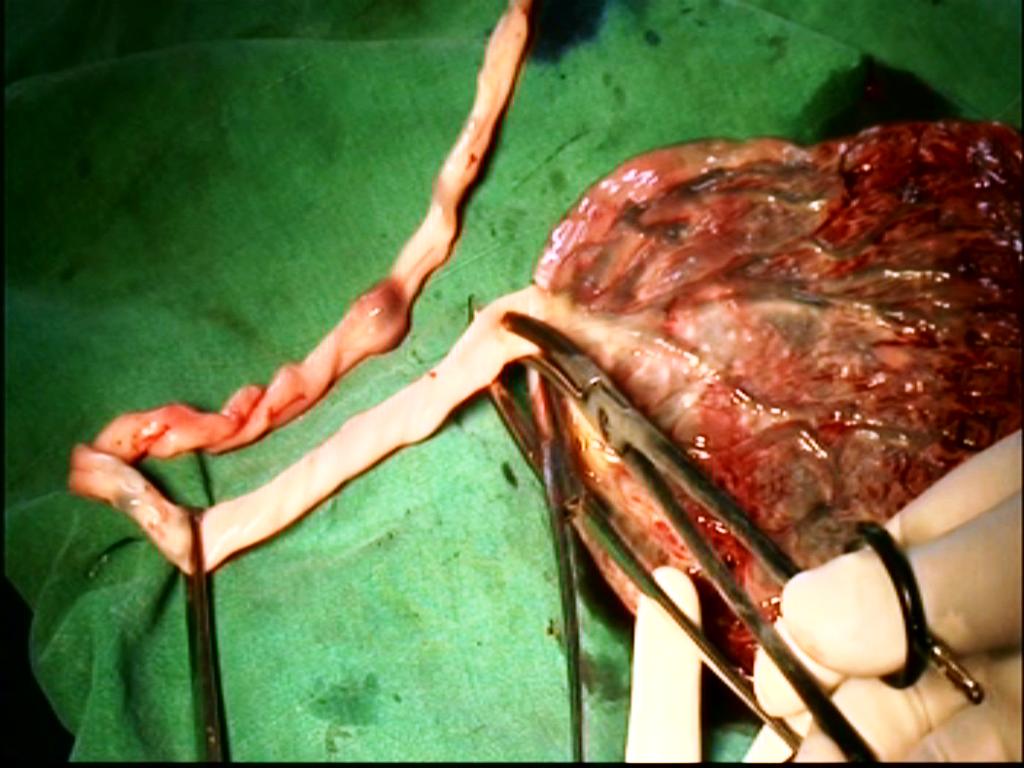
Salpingo oophorectomy at vaginal hysterectomy(Purohit technique).
Normal size uterus generally does not obstruct the accessibility to lateral pedicles. An enlarge uterus fills the pelvic cavity centrally and compresses drastically the lateral working space. It obstructs to the visibility and accessibility to the lateral pedicles to be secured. All lateral attachments of uterus are separated from the body to accomplish removal of uterus. Therefore, removal of the bulk is essential to increase the lateral space. Debulking is initiated when no further lateral pedicle is 'hooked' on sweeping the tip of forceps around the expanded lateral wall of uterus.
Uterus, larger than 12-14 weeks size invariably requires debulking. Only 10-15 % of cases had uterus above 12 weeks of gestation and 280 grams. Logically, the rest 85-90% cases would not require morcellation. Uterus up to 14-16 weeks sizes can be removed vaginally easily. Uterus size above the level of true pelvis may be carefully attempted by experienced surgeons. However, a standby facility for conversion to LAVH or laparotomy is needed to deal with failure cases. It is not wise to attempt vaginal hysterectomy on a uterus of above 20 weeks of gestation. Only 13.55% cases in our series required bisection and morcellation.Majority of uteri weighing less than 280 grams, did not require volume reduction maneuvers.
Bisection of cervix, myomectomy of visible myoma and wedge morcellation by knife and scissors of the directly visible bulk of the uterus are commonly practiced methods and enough to minimize or remove the centrally occupying obstruction to the lateral pedicles. In our experience, generally uteri weighing up to 300 grams do not require debulking. A soft uterus of 600 grams(Figure 5,6) has been removed intact by Purohit technique, for a right angle forceps can 'hook' a lateral pedicle from a tight working space and brings it to the mouth of bipolar forceps and scissors.It is the largest reported uterus removed intact vaginally during vaginal hysterectomy. When no further lateral pedicle is 'hooked' on sweeping the tip of forceps around the expanded lateral wall of uterus debulking is initiated (indication of debulking).

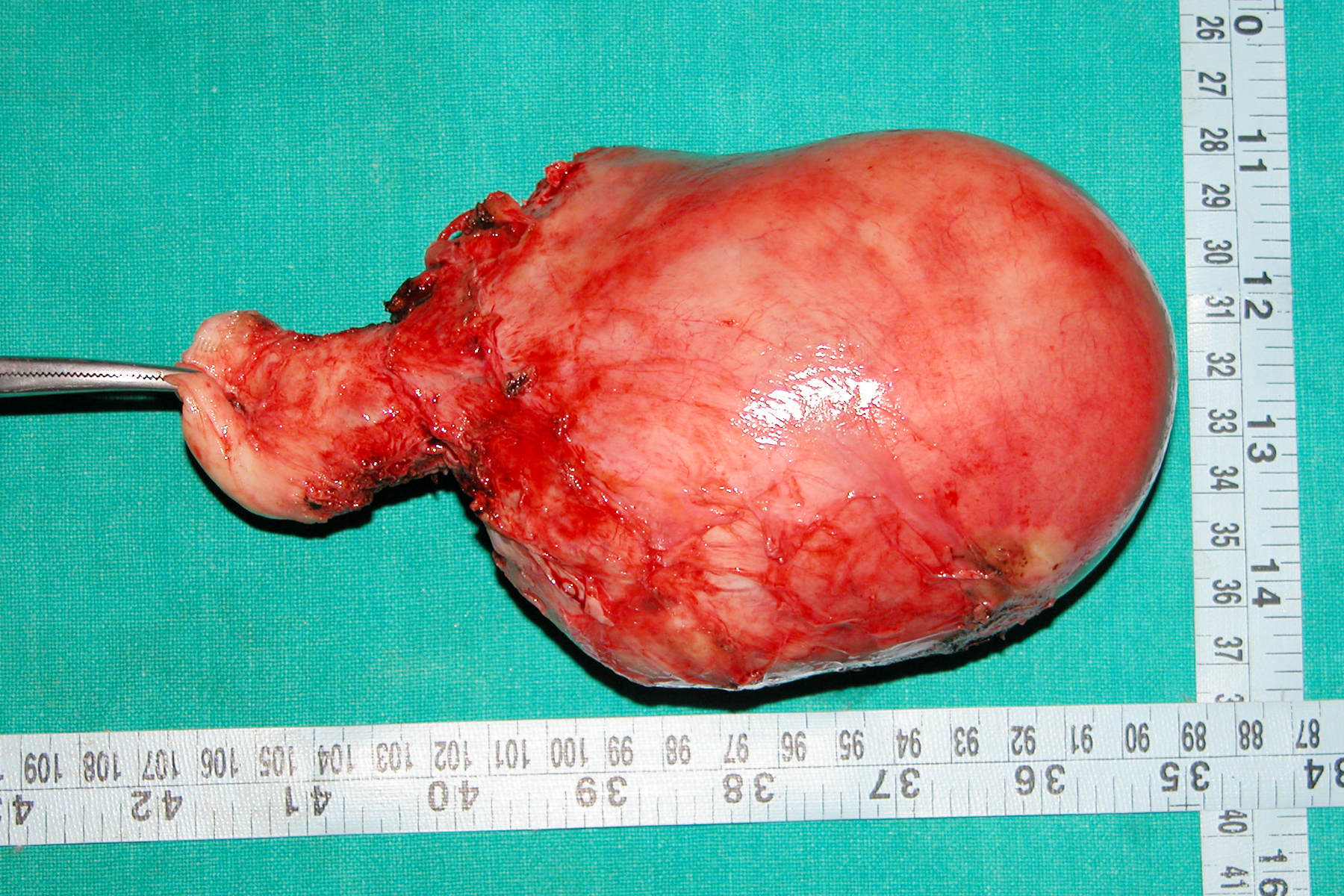
Figure 5,6.(16 weeks size and 600 grams uterus removed intact by Purohit technique)
Only13.55% cases required volume reduction maneuvers when Purohit technique was used in contrast to more than 30%
cases by conventional techniques Lash procedure of intramyometrial coring is available for moderate size uterus and
in a case with suspected endometrial carcinoma where uterine cavity is kept intact. With the development of Purohit
technique a moderate size uterus may be removed intact thus, coring was not needed.
Volume reduction maneuvers are normally carried out after bilateral ligation of uterine arteries. Hemorrhage is expected in conducting debulking before ligation of uterine arteries in cases of large cervical polyp, big central cervical fibroid and requires blood transfusion. Smaller ones do not cause problems thus can be attempted. Intracapsular morcellation of myoma removes the fear of injury to the neighboring tissues.
Success of the debulking procedure depends on the successive descent of the uterus to the surgeon's view in response to the removal of wedges and traction. Solid big firm myoma occupying above the level of true pelvis and sitting above the brim does not descend adequately following morcellation and consumes lots of time, energy, and patience. Soft cystic degenerated myoma following debulking responses well to the traction and descend faster towards the surgeon. A funnel type below upwards expansion of uterus is better for debulking than umbrella type expansion of fundus with a long stalk below. A big pedunculated fundal fibroid with a long stalk some time does not come out with uterus and often needs traction and debulking.
Conclusions:
INTRAOPERATIVE COMPLICATIONS:
Blood transfusion: Rarely required.
Be prepared for transfusion if the size of the uterus is more than 18 weeks and if the size of cervical fibroid is, more than 7-8 cm for it requires exhaustive morcellation, and sometime before ligation of at least one uterine artery.
Bladder injury-
In our extraperitoneal technique of bladder separation from the cervix and anterior wall of uterus, cystostomy is suspected when the finger enters in to a smooth empty space of bladder lumen and plenty of fluid floods the field on removal of finger.Hold the incised margins and repair in layers.
Rectal injury, bowel injury or ureter injury: we have not faced such injuries until today.
POSTOPERATIVE COMPLICATIONS:
Vault hematoma
We have seen in few cases during the early part of our study. Patient continues severe pelvic pain even after 48 hours. Ultrasonography of pelvis shows pelvic hematoma.Vault hematoma has been minimized; by routine tracing of the incised edge of posterior leaf of broad ligament up to the upper pedicles to check proper hemostasis, after routine use of our technique of vault closer and lavage of the pelvic cavity with Normal saline at the end of vaginal vault closer.No case of vault hematoma is seen after 2007.However, the vault hematoma is drained under transabdominal sonographic guidance after filling bladder with about 300 ml normal saline.Best way to deal with pelvic hematoma is-go for three ports laparoscopy. Examine the pelvic cavity and stumps for hematoma. Do a lavage with normal saline. No cauterization is needed.
Small burn injury to vulval skin and labia minora-Inner side of the vaginal skin and labia minora are occasionally trapped between the prongs of the activated bipolar forceps with broken insulation and are cauterized without the intention of surgeon. Thus, do not use bipolar forceps with broken insulation beyond its active tip or be careful. The patient with a small burn ulcer complains of burning during micturation. It is treated with adequate antibiotic ointment. Ask her to apply ointment before she intends to pass urine. It heals in few days.
Bleeding from vaginal vault-
We have not seen postoperative bleeding from uterine artery.Occasionally a phone call is received at the end of one month after operation saying, few drops of blood came out of vagina.It usually comes from suture points of vault mucosa. It usually stops on its own. No treatment other than haemostatic drug is required. In one case out of initial 680, we had to cauterize a tiny arteriole at the suture line of vaginal vault.
Vaginal discharge:
It remains until suture materials are there at the vaginal vault. It stops on its own. No special treatment is required. Lavage of the pelvic cavity with Normal saline after closer of vaginal vault drastically reduces the fetid smell and thickness of the vaginal discharge.
Postoperative pyrexia occurs mostly due to cystitis. Vault infection is also rarely seen.
Vault granulation
very rare and are cauterized if needed
Vault prolapse:
We have seen four cases of vault prolapse in the initial 680 cases before 2005. In all cases cystocele occurred with in one year of vaginal hysterectomy. After 2005 and after adopting our technique of vault plication suture as described above, vault prolapsed has been minimized.
POSTOPERATIVE MANAGEMENT:
Routine prophylactic antibiotic, anti emetic (Ondansetron), Ranitidine IV fluid 12 hours, Oral fluid after 3 hours, Catheter removal after 12 hours, Vaginal drain (Ryle's tube) removal after 6-8 hours, Solid diet after 12 hours, Analgesic for minimum 12 hours then if needed. Patient can go home after 24-36 hours of operation, if she feels comfortable with oral antibiotics, analgesic, antacid, and laxative, multivitamins. She is told to have mild vaginal discharge for few days, mild lower abdominal discomfort for few days. She is advised to telephone if any problem occurred.She may join work once she gains her confidence. Postoperative check up after one month. Anaesthesia during operation - we prefer spinal anaesthesia
To watch the video, kindly register and note the Username and Password for future log in. You can also download the video to your computer. To learn and practice, always watch the steps of the procedure before entering the operation theater for vaginal hysterectomy at least for six months. Kindly see some interesting specimens removed during vaginal hysterectomy by Purohit technique and appreciate the scope of the technique. We request you to kindly fill up the feedback form or email your comments and suggestions on different aspects of the technique, which will be valuable for us.
Note:
Declaration:
©All rights reserved with Purohit General Hospital and research center.
Updated as on date 30/06/2012
References.
-
- Ram Krishna Purohit: Purohit technique of vaginal hysterectomy:
- a new approach BJOG (British Journal of Obstetric and Gynaecology):
- an International Journal of Obstetrics and Gynaecology, 2003 Dec, Vol. 110 (12) pp. 1115-1119
- View this document:To download right click and select save link as
- Ram K. Purohit: Purohit technique of vaginal hysterectomy:
- A new approach performed in 214 patients.
- Gynaecological endoscopy 2002 Dec; 11(6); 423-430
- View this document:To download right click and select save link as
- R. K. Purohit, A. K. Pattnaik:
- Vaginal Hysterectomy by Electrosurgery (An Extraperitoneal Approach),
- J Obstet Gynecol India Vol.51, No. 5: September/October 2001 Pg 162-164
- View this document:To download right click and select save link as
- Purohit Ram Krishna, Tripathy Prakash Narayan, Pattnaik Abhaya Kumar:
- Vaginal Hysterectomy Using Electrocautery and Purohit Approach To Uterine Artery,
- J Obstet Gynecol India Vol.53, No. 5: September / October 2003 Pg 475-478
- View this document:To download right click and select save link as
- Ram Krishna Purohit, MD, Jay Gopal Sharma, MS, Sarabjeet Singh, DGO, and Dipak Kumar Giri, MD:
- Vaginal Hysterectomy by Electrosurgery for Benign Indications Associated with Previous Cesarean Section
- JOURNAL OF GYNECOLOGIC SURGERY Volume 29, Number 1, 2013, Pages: 07 - 12 © Mary Ann Liebert, Inc.DOI: 10.1089/gyn.2012.0082
- View this document:To download right click and select save link as
- Ram Krishna Purohit, MD, Jay Gopal Sharma, MS and Shikha Joshi, MD:
- Adnexectomy During Vaginal Hysterectomy for Benign Indications Using Bipolar Hemostasis of Lateral Pedicles and Transvaginal Adnexa Mobilization
- JOURNAL OF GYNECOLOGIC SURGERY Volume 31, Number 2, 2015 Pages: 86 - 91 © Mary Ann Liebert, Inc.DOI: 10.1089/gyn.2014.0088
- View this document:To download right click and select save link as
- Ram Krishna Purohit, MD, Jay Gopal Sharma,Devajani Meher,Sanjay Raosaheb Rakh and Surya Malik:
- Completion of vaginal hysterectomy by electro surgery using anteroposterior approach in benign cases faced with obliterated posterior cul-de-sac
- View this document:To download right click and select save link as
- Dr.Ramkrishna Purohit,Dr.Jay Gopal Sharma,Dr.Devajani Meher,Dr.Sanjay Raosaheb Rakh,Dr.Minal Choudhary:
- A laparovaginal strategy to avoid bladder injury during laparoscopic-assisted vaginal hysterectomy in cases with ventrofixed uterus following previous cesarean section
- International Journal of Women’s Health
- View this document:To download right click and select save link as